Holistic Care Elements
We strive to help our patients become ‘Symptom-free, Drug-free & Doctor-free©’. Our specialists have many years of experience in treating patients. Following an initial consultation, they will put together a detailed tailor-made programme to best address the patient’s care.
The multi-disciplinary approach means that the treatment might include a variety of lifestyle, nutritional, and exercise care. In some cases, the treatment may consist of a drug prescription. The focus of the care is reverse disease.
The impact of treatment is regularly assessed to ensure that results align with treatment.
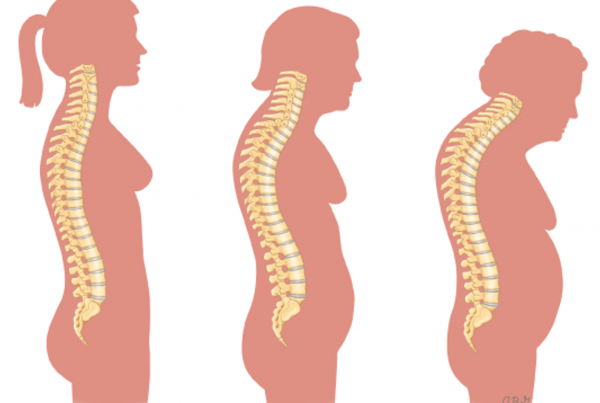
These suggestions may help reduce your risk of developing osteoporosis or experiencing broken bones:
- Avoid smoking. Smoking increases bone loss, perhaps by decreasing the amount of oestrogen a woman’s body makes and by reducing calcium absorption in the intestine.
- Avoid excessive alcohol. Consuming more than one alcoholic drink daily may decrease bone formation and reduce the body’s ability to absorb calcium. Being under the influence also can increase the risk of falling.
- Prevent falls. Wear low-heeled shoes with non-slip soles, and check the house for hazards that might cause you to trip or fall. Keep rooms brightly lit, install grab bars inside and outside your shower door, and ensure you can quickly get in and out of your bed.
Nutrition plays a crucial role in preventing the development of osteoporosis, but many people aren’t aware that food also aids treatment. It plays such a vital role that drug treatment and other interventions are rendered less effective without adequate nutrition. After all, to form new bone tissue, your body requires certain raw materials to work with. This includes minerals like calcium, magnesium, and phosphorus.
These essential nutrients are needed daily to enhance bone growth.
- Vitamin D
Vitamin D is essential for helping your body absorb the calcium in your food. Doctors can quickly assess a patient’s levels via a simple blood test. Margarine, cereals, and even some dairy products have vitamin D added to them. Then, some foods naturally contain vitamin D, such as fatty fish and eggs. Multi-vitamin supplements can help improve the body’s vitamin D levels. Ten minutes of sunlight per day is also recommended. (Graphic Credit: PharmaNord 2015) - Calcium
It is vital for bone health and is also needed for muscle contraction, heartbeat rate and the blood clotting mechanism. Along with consuming the required amount of calcium daily, your body can only use it if your other needs are met. Find out more here. - Protein
Our bodies require a healthy protein intake throughout our lives to sustain our muscle strength, which helps bone density and reduces the risk of falls. - Magnesium
Magnesium, another essential mineral, helps with calcium absorption and metabolism. Studies show that supplementing the diet with magnesium can help prevent bone fractures in people. Furthermore, it’s also essential for muscle contraction and many other functions, all of which contribute to adequate bone health and tissue formation.
If you think you or your family are at risk of osteoporosis or have osteoporosis, there are several new treatment approaches to cut the risk of future fractures and complications.
For more nutritional information, we offer this free educational programme.
The most essential nutrients for bone health include calcium, vitamin D, protein, and magnesium.
Exercise is essential to prevent osteoporosis. Studies prove that weight-bearing exercise can help increase bone density levels by increasing muscle mass. We recommend bringing diversity to your exercise routine to benefit your bones and muscles. Different kinds of movements in multiple directions and at different speeds can prove beneficial.
Each one is carefully considered following a thorough patient assessment.
For both men and women, the most widely prescribed osteoporosis medications are bisphosphonates. Examples include:
- Alendronate (Fosamax)
- Risedronate (Actonel)
- Ibandronate (Boniva)
- Zoledronic acid (Aclasta, Zometa)
Injected forms of bisphosphonates don’t cause stomach upset. And it is easier to schedule a quarterly, six monthly or yearly injection than to remember to take a weekly or monthly pill.
Hormone-related therapy (HRT)
Oestrogen, especially when started soon after menopause, can help keep up bone density. However, as with all drug treatments, the side effects need to be considered. Raloxifene (Evista) mimics oestrogen’s beneficial effects on bone density in postmenopausal women without some of the risks associated with oestrogen.
In men, osteoporosis may be linked with a gradual age-related decline in testosterone levels. Testosterone replacement therapy can help increase bone density, but osteoporosis medications are preferred instead of or in addition to testosterone.
Less common osteoporosis medications
If you can’t tolerate the more common treatments for osteoporosis — or if they don’t work well enough — these alternatives are available:
- Teriparatide (Forteo). This powerful drug is similar to parathyroid hormone and stimulates new bone growth. It is given by injection under the skin.
- Denosumab (Prolia). Compared with bisphosphonates, denosumab produces similar or better bone density results while targeting a different step in the bone remodelling process.
We offer educational programmes aimed to help you improve your health. Find out more
© 2024 London Osteoporosis Clinic. Made by Connecting Matrix.