Osteonecrosis of the Jaw (ONJ) is a complex and relatively rare condition that has garnered significant attention due to its association with certain medications and specific risk factors. In this comprehensive discussion, we will delve deeper into the risk factors, medical conditions leading to ONJ, and the medications, particularly bisphosphonates, that may contribute to its development.
Understanding the Risk Factors
- Bisphosphonate Medications: Among the foremost risk factors for ONJ are bisphosphonate medications. These drugs, which include alendronate (Fosamax), risedronate (Actonel and Atelvia), ibandronate (Boniva), zoledronic acid (Reclast), and denosumab (Prolia), are commonly prescribed to manage conditions such as osteoporosis. The precise mechanism by which bisphosphonates raise the risk of ONJ is not fully elucidated. Still, theories suggest they may disrupt the bone’s natural healing processes, inhibit blood vessel formation, or increase infection susceptibility. It’s important to note that the risk of ONJ occurring in individuals taking these medications remains very low but may be slightly elevated in those who require invasive dental procedures while on bisphosphonate therapy.
- Invasive Dental Procedures: The need for invasive dental procedures, such as dental extractions or dental implant placements, can contribute to ONJ risk, especially in individuals concurrently taking bisphosphonates. Dentists and healthcare providers should carefully evaluate the necessity and potential risks associated with such procedures in patients with a history of bisphosphonate use.
- Cancer Treatment: Patients undergoing cancer treatment with intravenous bisphosphonates are at a higher risk of developing ONJ compared to those receiving lower doses for osteoporosis management. The increased risk in cancer patients is likely attributed to the higher amounts and frequency of bisphosphonate administration as part of their cancer therapy.
- Age: Age plays a significant role in ONJ risk. Older individuals are generally more susceptible to bone-related complications, including ONJ. The natural ageing process can impact bone health, making older patients more vulnerable to this condition.
- Medical Conditions: Certain medical conditions, such as diabetes, can increase the likelihood of ONJ development. Diabetes can impair the body’s ability to heal effectively, which can contribute to the onset of ONJ in susceptible individuals.
- Gum Disease and Smoking: Pre-existing gum disease and smoking are additional factors that heighten the risk of ONJ. Both of these conditions can compromise oral health, exacerbating the effects of bisphosphonate medications on the jawbone’s health.
Recognising Signs and Symptoms of ONJ
Early recognition of ONJ is paramount for timely intervention and effective management. Patients with ONJ may exhibit the following signs and symptoms:
- Persistent Pain: Patients often report constant pain in the jaw or mouth region, which may be localized or more widespread.
- Soft Tissue Swelling: Swelling of the soft tissues within the oral cavity, particularly around the affected area.
- Drainage: Oozing or drainage from the site of ONJ can be a sign of infection or tissue breakdown.
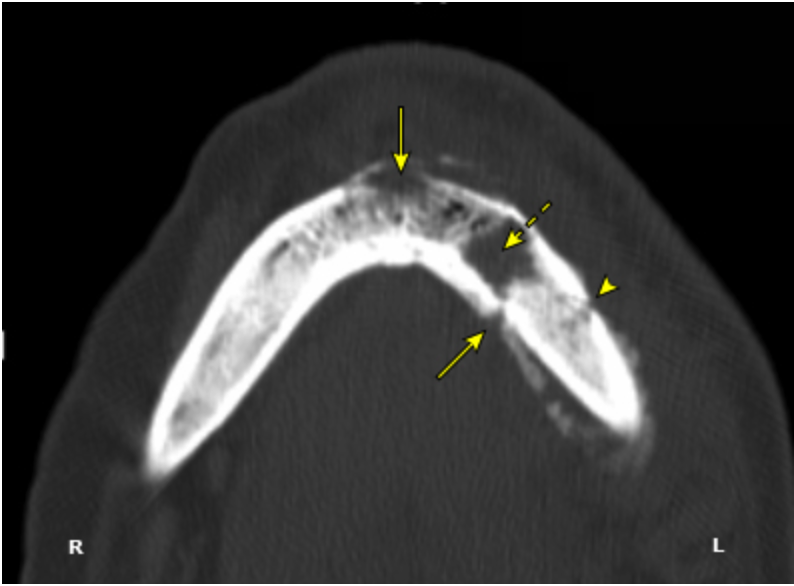
- Exposed Jawbone: One of the hallmark signs of ONJ is the exposure of the jawbone, as it is no longer adequately covered by the gums.
- Bad Breath: Patients may experience unpleasant breath odour, often associated with infection or tissue degradation.
- Loose Teeth: Teeth in the vicinity of ONJ may become loose or feel unstable due to the compromised integrity of the jawbone.
- Signs of Infection: Signs of infection on the gums, such as redness, swelling, or pus, may be evident in cases of ONJ.
Common Treatments for ONJ
Patients diagnosed with ONJ, especially those with underlying osteoporosis, typically receive conservative treatments to manage the condition. These treatments may include:
- Oral Rinses: The use of antiseptic oral rinses to promote oral hygiene and reduce the risk of infection.
- Antibiotics: Antibiotics are often prescribed to manage or prevent infections in the affected area. Infections can exacerbate the symptoms of ONJ.
- Oral Analgesics: To alleviate the discomfort associated with ONJ, patients may be given oral analgesics or pain-relieving medications.
Surgical intervention is generally not recommended for ONJ due to the potential for interfering with the compromised bone healing process.
The Role of a Rheumatologist
In cases where ONJ is a concern, particularly for individuals at risk due to medication or underlying medical conditions, consulting a rheumatologist can be invaluable. Rheumatologists specialise in treating osteoporosis with antiresorptive drugs and have expertise in managing the risk of ONJ. Their guidance can help patients receive appropriate care and risk mitigation strategies.
Conclusion
Osteoporosis drugs, particularly bisphosphonates, are a crucial factor contributing to developing Osteonecrosis of the Jaw (ONJ). Understanding the risk factors, signs and symptoms, and appropriate treatment approaches for ONJ is essential for healthcare providers to provide the best possible care for their patients, particularly those at higher risk due to medication or underlying medical conditions. By remaining informed and proactive, we can contribute to the overall well-being of individuals at risk of ONJ.
For further information on bone health and related topics, please visit our website at LondonOsteoporosisClinic.com.